Frequently Asked Questions
Updated on February 4, 2022
We are drawing this information from the websites of a variety of trustworthy organizations (e.g. World Health Organization (WHO), the United States Centers for Disease Control and Prevention (CDC), the Ministry of Health and Family Welfare, (MoHFW) Government of India, the Indian Council of Medical Research (ICMR) and the Cleveland Clinic among others). Some of this language is used word for word, and other language is paraphrased. We would like to acknowledge the hard work of these organizations in compiling this information.
Important terms:
WHO: World Health Organization
CDC: United States Centers for Disease Control and Prevention
COVID-19: COVID-19 is a new disease, caused by a novel (or new) coronavirus (SARS-CoV-2) that has not previously been seen in humans. There are many types of human coronaviruses including some that commonly cause mild upper-respiratory tract (sinuses, nasal passages, pharynx and larynx) illnesses. In COVID-19, ‘CO’ stands for ‘corona,’ ‘VI’ for ‘virus,’ ‘D’ for ‘disease’ and ‘19’ for ‘2019.’
Getting a vaccine- eligibility, vaccine timing, and doses
Who is eligible for the COVID-19 vaccine?
UPDATED As of 3rd January 2022, children in the age-group 15-18 years and all adults over 18 years (including pregnant and lactating women) are eligible for the COVID-19 vaccine. However, only “Covaxin” is the approved vaccine for children in the age-group 15-18 years. Please check your local state guidelines for more information.
If you cannot pre-register online, please contact your local government health workers, who will refer you to the government COVID-19 Vaccination Center for on-the-spot registration, appointment, verification, and vaccination on the same day.
For more information, please visit: https://www.mohfw.gov.in/covid_vaccination/vaccination/faqs.html, https://www.mohfw.gov.in/pdf/FAQsCOVID19vaccinesvaccinationprogramWebsiteupload.pdf and https://www.mohfw.gov.in/pdf/GuidelinesforCOVID19VaccinationofChildrenbetween15to18yearsandPrecautionDosetoHCWsFLWs&60populationwithcomorbidities.pdf
Who is eligible for the COVID-19 vaccine precaution dose?
NEW As of 10th January 2022, Health Care Workers and Front-Line Workers who have received two doses of the COVID-19 vaccine are eligible to receive another dose of the vaccine called the precaution dose. All persons aged 60 years and above with comorbidities and who have received two doses of the COVID-19 vaccine are eligible to receive the precaution dose based on their doctor’s advice. The order in which these precaution doses would be given are based on the completion of 9 months or 39 weeks from the second dose.
For more information, please visit: https://www.mohfw.gov.in/pdf/GuidelinesforCOVID19VaccinationofChildrenbetween15to18yearsandPrecautionDosetoHCWsFLWs&60populationwithcomorbidities.pdf
If I have already had COVID-19 and recovered, do I still need to get the COVID-19 vaccine?
Yes, you should get a COVID-19 vaccine, even if you’ve had COVID-19. The vaccine will still help in developing a strong immune response against the disease. But wait for 3 months after being infected with COVID-19 before getting the vaccine.
We do not know yet if people who have had COVID-19 will have enough of an immune response to protect them from getting COVID-19 again. Even if there is some protection, it is not known how long it will last. This is why people who have had COVID-19 should still get a COVID-19 vaccine.
For more information, please visit: https://www.mohfw.gov.in/covid_vaccination/vaccination/faqs.html
If I currently have COVID-19, should I get the vaccine now?
No, people with confirmed or suspected COVID-19 should be in isolation for at least 10 days. Having infected people at the vaccination site would increase the risk of spreading the virus. Since people with COVID-19 develop some immunity against the disease, the Ministry of Health and Family Welfare, Government of India (MoHFW, GoI) recommends deferral of vaccination for 3 months after recovery.
What if I get COVID-19 in between 2 vaccine doses?
For most people who have 1 dose of the vaccine, the disease is likely to be mild or moderate, depending on how many days after vaccination the virus exposure happens. If exposure occurs within 1 to 3 weeks of getting the first dose (of Covaxin or Covishield), the vaccine is unlikely to have an effect and is not expected to change the course of the infection. However, if a person tests positive after 3 weeks from their first dose, they are highly likely to only get a mild case of COVID-19.
Once a person gets COVID-19, their body starts producing antibodies to it. Therefore, experts suggest waiting 3 months after recovering from COVID-19 before getting the second dose. Getting the second dose is important to ensure an effective immune response against COVID-19 in the future.
So, while experts learn more and as people get vaccinated, it is important for everyone (vaccinated and unvaccinated) to continue wearing masks, washing our hands, and keeping physical distance from others to help stop this pandemic.
For more information, please visit: https://www.mohfw.gov.in/covid_vaccination/vaccination/faqs.html
Why do I need to get two doses of the vaccine?
Recent studies have shown that certain time frames between vaccine doses allow for the best immune response. This timing is different for each vaccine. This has to do with the different ways each vaccine works with your body’s immune system.
Covishield: Real-world studies of the Covishield vaccine show that waiting a longer time between doses led to a better immune response. So the time between the two doses has been increased to 12-16 weeks.
Covaxin: Scientists recommend that the second dose of the Covaxin vaccine be taken 4-6 weeks after the first dose.
For more information, please visit: https://www.mohfw.gov.in/covid_vaccination/vaccination/faqs.html
What is the right timing between COVID-19 vaccine doses?
Recent studies have shown that certain time frames between vaccine doses allow for the best immune response. This timing is different for each vaccine. This has to do with the different ways each vaccine works with your body’s immune system.
Covishield: Real-world studies of the Covishield vaccine show that waiting a longer time between doses led to a better immune response. So the time between the two doses has been increased to 12-16 weeks.
Covaxin: Scientists recommend that the second dose of the Covaxin vaccine be taken 4-6 weeks after the first dose.
For more information, please visit: https://www.mohfw.gov.in/covid_vaccination/vaccination/faqs.html
Do I need to get the same vaccine for the first and second dose of my COVID-19 vaccine?
Yes. The vaccines currently available in India are not interchangeable. So, you need to get the same second dose of the vaccine as the first one. Your vaccine registration (through the CoWIN portal) is also going to help to ensure that you get the same vaccine for both doses.
For more information, please visit: https://www.mohfw.gov.in/covid_vaccination/vaccination/faqs.html
Getting a vaccine- during and after your appointment
How can I stay safe from COVID-19 at vaccination centers?
- Keep at least 6 feet (2 meters) distance from others at the center.
- Wear a 3-layered medical mask or N95 mask over your nose and mouth. If not possible, double mask (wear a cloth mask over a disposable surgical mask).
- Do not touch your face or any surfaces. Do not shake hands.
- Sanitize your hands often.
- Avoid talking to others.
- Plan ahead. Register in advance, if possible, and understand the timing of your next appointment.
- Stay at home and reschedule your appointment if you have symptoms for COVID-19, or, have COVID-19.
For more information, please visit: https://www.mohfw.gov.in/covid_vaccination/vaccination/faqs.html
Do I need to wear a mask and avoid close contact with others if I have received two doses of the vaccine?
Yes. While experts learn more about the protection that COVID-19 vaccines provide under real-life conditions, it will be important for everyone to continue using all the tools available to us to help stop this pandemic. These tools include covering your mouth and nose with a mask, washing hands often, and staying at least 2 meters away from others. Together, the COVID-19 vaccine and everyone following the COVID-19 safety guidelines will offer the best protection from getting and spreading COVID-19. Experts need to understand more about the protection that COVID-19 vaccines provide before deciding to change recommendations on steps everyone should take to slow the spread of the virus that causes COVID-19.
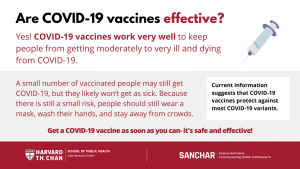
COVID-19 vaccines are effective at preventing COVID-19 disease, especially severe illness and death. But we’re still learning how well COVID-19 vaccines keep people from spreading the disease. Moreover, we’re still learning how effective the vaccines are against variants of the virus that causes COVID-19. Early data show the vaccines may work against some variants but could be less effective against others.
A small number of people may still develop infection, but it is likely to be less severe. And hence it is necessary to wear a mask, wash hands and stay away from crowds. Until we know more about the effectiveness of the vaccine against the variants, and until a majority of the population is vaccinated to reach herd (or community) immunity, it is necessary to continue to follow the COVID-19 prevention protocols.
Source: https://www.mohfw.gov.in/covid_vaccination/vaccination/faqs.html
https://www.cdc.gov/coronavirus/2019-ncov/vaccines/fully-vaccinated.html
Are there side effects to receiving the vaccine?
COVID-19 vaccination will help protect you from getting COVID-19. You may have some side effects, which are normal signs that your body is building protection. Common side effects include pain and swelling at the site of injection, and flu-like symptoms such as fever, chills, tiredness and headache. These should go away in a few days.
It has been seen that some people can develop allergic reactions after getting the COVID-19 vaccine. If you have ever had a severe allergic reaction to other vaccines or injectables, it is recommended that you speak to your doctor before getting vaccinated.
Do fully vaccinated people in India need to continue wearing masks in social settings?
Yes. While experts learn more about the protection that COVID-19 vaccines provide under real-life conditions, it is important for everyone to continue using all the tools available to help stop this pandemic. These tools include covering your mouth and nose with a mask, washing hands often, and staying at least 6 feet or 2 meters away from others. Together, the COVID-19 vaccine and everyone following COVID-19 safety guidelines will offer the best protection from getting and spreading COVID-19.
COVID-19 vaccines are effective at preventing COVID-19 disease, especially severe illness and death. But we are still learning how well COVID-19 vaccines keep people from spreading the disease. We are also still learning how effective the vaccines are against variants of the COVID-19 virus (variants are versions of the virus with slight changes, or mutations, that sometimes affect how contagious or severe the virus can be). Early data show the vaccines may work against some variants but could be less effective against others.
Experts need to understand more about the protection that COVID-19 vaccines provide before deciding to change recommendations on what everyone should do to slow the spread of COVID-19. So, while experts learn more and as people get vaccinated, it is important for everyone to continue wearing masks, washing our hands, and keeping physical distance from others to help stop this pandemic.
Adapted from: https://www.mohfw.gov.in/covid_vaccination/vaccination/faqs.html
https://www.cdc.gov/coronavirus/2019-ncov/vaccines/fully-vaccinated.html
Vaccine Safety
Can I get COVID-19 from the vaccine?
No, the different types of vaccines have different materials in them that will signal our bodies to produce the proteins or antibodies to protect us from the virus. NONE of these vaccines contain the active virus.
The immune response that is initiated in the body might lead to symptoms, such as fever. This does not mean the person is infected with the virus. Learn more on how Covishield (Serum Institute) and Covaxin (Bharat Biotech) vaccines work.
It typically takes a few weeks for the body to build immunity after vaccination. That means it’s possible a person could be infected with the virus that causes COVID-19 just before or just after vaccination and get sick. This is because the vaccine has not had enough time to provide protection.
How do we know the vaccine is safe?
The most commonly used vaccines we have today have been in use for decades, with millions of people receiving them safely every year. As with all these successful vaccines, COVID-19 vaccines have also undergone extensive and rigorous testing before being approved. Scientists around the world have been working since early 2020 to develop the current possible COVID-19 vaccines and go through all of the testing processes to ensure they are safe. The vaccine safety is also monitored after the vaccines have been introduced which is called post-market surveillance. This ensures that the vaccines will continue to meet the same quality, safety and performance requirements as when they were initially introduced in the market.
Is it safe for me to get the vaccine if I am pregnant or breastfeeding?
The vaccines being used under the national vaccination program are found to be safe and effective. Based on how these vaccines work in the body, experts believe they are unlikely to pose a risk for people who are pregnant. The National Technical Advisory Group on Immunization (NTAGI) has recommended that “pregnant women may take any one of the two Covid-19 vaccines and lactating women are also eligible for jabs at any time before and after delivery.” This recommendation is based on the emerging evidence which shows that benefits of COVID-19 vaccination during pregnancy far outweigh the risk associated with contracting COVID infection during pregnancy (like increased risk for severe illness, preterm birth). However, it’s important that pregnant women make an informed choice.
For more information, please visit: https://www.mohfw.gov.in/pdf/FAQsCOVID19vaccinesvaccinationprogramWebsiteupload.pdf
Are risks of COVID-19 vaccination more than its benefits for a pregnant/lactating woman?
No, the very real benefits of vaccinating pregnant and lactating women seem to far outweigh any theoretical and remote risks of vaccination. Lactating women are also considered for Covid vaccine as there are no known adverse effects on the neonate who is breastfeeding. In fact, there is a possibility of passage of protective antibodies to the child, which may have a beneficial effect.
For more information, please visit: https://www.mohfw.gov.in/pdf/FAQsCOVID19vaccinesvaccinationprogramWebsiteupload.pdf
Which vaccines should I take if I am pregnant?
National Technical Advisory Group on Immunization (NTAGI) recommends that pregnant women may take any one of the two Covid-19 vaccines (Covishield or Covaxin). You must consult your doctor about the choice of vaccine in particular case. Both COVISHIELD and COVAXIN can be used during pregnancy or lactation.
For more information, please visit: https://www.mohfw.gov.in/pdf/FAQsCOVID19vaccinesvaccinationprogramWebsiteupload.pdf
Can women who are taking contraceptives and women planning to get pregnant get vaccinated?
Yes, women taking contraceptives can certainly get vaccinated. Pregnant women fall in the vulnerable group in terms of risk of serious disease in case of exposure. It might be safer to be fully immunized before conceiving.
For more information, please visit: https://www.mohfw.gov.in/pdf/FAQsCOVID19vaccinesvaccinationprogramWebsiteupload.pdf
Does getting the vaccine affect my future fertility and the chances of getting pregnant?
No, there is no evidence or no indications so far that the COVID vaccines impact fertility.
For more information, please visit: https://www.mohfw.gov.in/pdf/FAQsCOVID19vaccinesvaccinationprogramWebsiteupload.pdf
What should pregnant woman consider before getting the vaccine?
Expectant woman may consider discussing the following with their doctor/health care provider to guide them to make their decision:
- Likelihood of exposure to COVID-19, risks of COVID-19 to them and potential risks to her and fetus
- Benefits of getting vaccinated
- Information about the type of vaccine and known side effects of the vaccine.
For more information, please visit: https://www.mohfw.gov.in/pdf/FAQsCOVID19vaccinesvaccinationprogramWebsiteupload.pdf
What are the reasons someone should not get the COVID-19 vaccine?
There are a few contraindications or reasons why someone should talk to a doctor before getting a COVID-19 vaccine:
- If people have a history of:
- Anaphylactic or allergic reaction to a previous dose of COVID-19 vaccine
- Immediate or delayed-onset anaphylaxis or allergic reaction to vaccines or injectable therapies, pharmaceutical products/medicines, food items, etc.
- Pregnancy:
- Pregnant women have not been part of any COVID-19 vaccine clinical trial so far. Therefore, women who are pregnant or not sure of their pregnancy status should not get a COVID-19 vaccine at this time. As more data emerges, this may change.
- Temporary reasons to delay getting the COVID-19 vaccine are if someone:
- Had COVID-19 recently (vaccination should be delayed for 3 months after recovering from COVID-19)
- Has active symptoms of COVID-19 infection (get tested for COVID-19)
- Has COVID-19 and has been given monoclonal antibodies or convalescent plasma
- Is acutely unwell and hospitalized (with or without intensive care) due to any illness
After their illness is over and after an appropriate amount of time, someone who had one of these conditions can get a COVID-19 vaccine.
If you are not certain if you or someone in your household should get the vaccine, talk to
a doctor.
For more information, please visit: https://www.mohfw.gov.in/COVID_vaccination/vaccination/faqs.html
Are the COVID-19 vaccines protective against newer strains / mutated virus of SARS-CoV2?
The body responds to vaccination by making more than one type of antibodies to virus parts including spike protein. Therefore, vaccines continue to reduce a person’s risk of contracting the virus that cause COVID-19, including the Delta variant. Vaccines are highly effective against severe illness, but the Delta variant causes more infections and spreads faster than earlier forms of the virus that causes COVID-19.
Top Things You Need to Know:
- Variants are expected. The best way to slow the emergence of new variants is to reduce the spread of infection by taking measures to protect yourself including getting a COVID-19 vaccine when available.
- Vaccines keep you from getting sick, being hospitalized, or dying from COVID-19.
- All COVID-19 tests can detect all variants, but they will not tell you which variant you have.
For more information: https://www.cdc.gov/coronavirus/2019-ncov/variants/variant.html and https://www.mohfw.gov.in/pdf/FAQsCOVID19vaccinesvaccinationprogramWebsiteupload.pdf
Why are people getting infected even after vaccination?
COVID-19 vaccines are effective. However, a small number of vaccinated people may still get COVID-19, but it is likely to be less severe. That is why it is still necessary to wear a mask, wash hands, and stay away from crowds.
Why a vaccinated person might get COVID-19:
- It’s possible a person could have been infected just before or just after vaccination. It typically takes about 2 weeks for the body to build protection after the second dose of vaccination. Thus, a person can get sick if the vaccine has not had enough time to provide protection.
- The virus that causes COVID-19 is evolving, and new variants of the virus are spreading. Current data suggest that COVID-19 vaccines offer protection against most variants. However, some variants might cause illness in some people after they are fully vaccinated.
- A small percentage of people who are fully vaccinated will still get COVID-19 if they are exposed to the virus that causes it. These are called “vaccine breakthrough cases.” This means that while people who have been vaccinated are much less likely to get sick, it may still happen. Experts continue to study how common these cases are.
The overall risk of hospitalization and death among fully vaccinated people will be much lower than among unvaccinated people with similar risk factors.
Should one avoid taking vaccine during and around menstruation?
UPDATED The time period around menstruation is no contraindication to taking vaccines and like other vaccines, COVID-19 vaccine can be taken at any time of the monthly period.
One study reported that women who received both doses of a COVID-19 vaccine in a single menstrual cycle found that their period arrived a few days late. However, their periods were back to normal after a couple of months, so the change was only temporary. Therefore, the study concluded that there is no population-level clinically meaningful change in menstrual cycle length associated with COVID-19 vaccination.
For more information, please visit: https://www.gavi.org/vaccineswork/how-covid-19-vaccines-affect-menstrual-cycle
and https://www.mohfw.gov.in/pdf/FAQsCOVID19vaccinesvaccinationprogramWebsiteupload.pdf
Does Covishield (Oxford/AstraZeneca) vaccine cause blood clots?
Covishield is NOT associated with an increased overall risk of blood clotting disorders. There have been very rare cases of unusual blood clots accompanied by low levels of blood platelets. They symptoms associated with the rare blood clots that require prompt medical treatment include: breathlessness; pain in the chest or stomach; swelling or coldness in a leg; severe or persistent headaches or blurred vision; or tiny blood spots under the skin beyond the site of the injection. One should seek urgent medical attention if they have any of these symptoms in the weeks after their injection.
Serious side effects from vaccines are rare but they do occur, with any vaccine and for any disease. However, we are witnessing the largest mass vaccination campaign in history. Given the high number of people being vaccinated and the attention focused on the vaccines and the pandemic, some rare reactions are to be expected. It remains to be seen if similar concerns will be raised over other COVID-19 vaccines, but given that AstraZeneca’s was the first to be approved and has been given to far more people than any others, any rare adverse events are more likely to show up simply because of the sheer volume of people to have received it.
Source: https://www.gavi.org/vaccineswork/what-blood-clotting-disorder-astrazeneca-vaccine-has-been-linked
Vaccine Basics-vaccine development and how they work
What are the ingredients in vaccines?
Today’s vaccines use only ingredients that are safe and effective. Each ingredient in a vaccine serves a specific purpose. For example, vaccine ingredients may:
- Help provide immunity (protection) against a specific disease
- Help keep the vaccine safe and long lasting
- Be used during the production of the vaccine
Ingredients provide immunity-
Vaccines include ingredients to help your immune system respond and build immunity to a specific disease. For example:
- Antigens are very small amounts of weak or dead germs that can cause diseases. They help your immune system learn how to fight off infections faster and more effectively. The flu virus is an example of an antigen.
- Adjuvants, which are in some vaccines, are substances that help your immune system respond more strongly to a vaccine. This increases your immunity against the disease. Aluminum is an example of an adjuvant.
- Messenger ribonucleic acid (mRNA), in some new COVID-19 vaccines, is the active component that generates an immune response in the recipient.
Ingredients keep vaccines safe and long lasting-
Some ingredients help make sure a vaccine continues to work like it’s supposed to and that it stays free of outside germs and bacteria. For example:
- Preservatives protect the vaccine from outside bacteria or fungus. Today, preservatives are usually only used in vials (containers) of vaccines that have more than 1 dose. That’s because every time an individual dose is taken from the vial, it’s possible for harmful germs to get inside. Most vaccines are also available in single-dose vials and do not have preservatives in them.
- Stabilizers, like sugar or gelatin, help the active ingredients in vaccines continue to work while the vaccine is made, stored, and moved. Stabilizers keep the active ingredients in vaccines from changing because of something like a shift in temperature where the vaccine is being stored.
Ingredients used during the production of vaccines-
Some ingredients that are needed to produce the vaccine are no longer needed for the vaccine to work in a person. These ingredients are taken out after production so only tiny amounts are left in the final product. The very small amounts of these ingredients that remain in the final product aren’t harmful. Examples of ingredients used in some vaccines include:
- Cell culture (growth) material, to help grow the vaccine antigens.
- Inactivating (germ-killing) ingredients, like formaldehyde, to weaken or kill viruses, bacteria, or toxins in the vaccine.
- Antibiotics, like neomycin, to help keep outside germs and bacteria from growing in the vaccine.
The claim that these vaccines contain a microchip or tracker is FALSE. The claim that these vaccines contain mercury is also FALSE.
Composition of Covishield includes inactivated adenovirus with segments of Coronavirus, Aluminium Hydroxide Gel, L-Histidine, L-Histidine Hydrochloride Monohydrate, Magnesium Chloride Hexahydrate, Polysorbate 80, Ethanol, Sucrose, Sodium Chloride, and Disodium Edetate Dihydrate (EDTA).
Composition of Covaxin includes inactivated Coronavirus, Aluminum Hydroxide Gel, TLR 7/8 Agonist, 2-Phenoxyethanol and Phosphate Buffered Saline [NKA1].
For more information about the ingredients and possible allergens, please ask your provider before getting the vaccine.
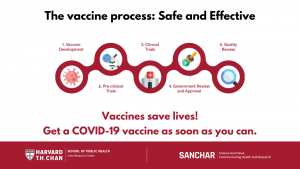
Why was the COVID-19 vaccine developed so much faster than other vaccines?
The vaccine process is happening faster because vaccine research and development, clinical trials, manufacturing, and plans for distribution are taking place at the same time. This method removes delays that occur when these processes are carried out one after the other. Steps to ensure safety have not been eliminated.
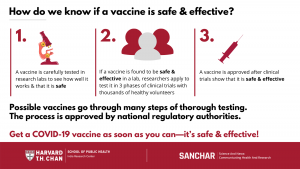
How are vaccines tested?
Vaccines go through an intensive testing process that includes careful examination of the vaccine and its ingredients. These tests evaluate the safety of the vaccine and how well it prevents a disease. Tests are first done in research labs, and then if the vaccine proves to be effective and safe, researchers can apply to start clinical trials.
Clinical trials typically involve several thousand healthy volunteers in three phases, with increasing numbers of participants in each phase. Trials in all phases have to follow strict safety regulations that are set by national regulatory authorities that prioritize participant safety. When vaccine manufacturers apply for approval for their vaccine, the results of all clinical trials are considered.
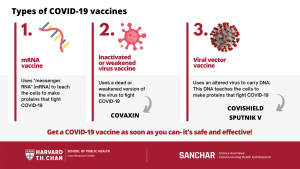
How do the different COVID-19 vaccines work?
Multiple COVID-19 vaccines are being developed, tested, and approved. They are all meant to teach the body’s immune system to safely recognize and block the coronavirus. The vaccine types include:
- Inactivated or weakened virus vaccines, which use a form of the virus that has been inactivated or weakened so it doesn’t cause disease, but still creates an immune response. For example: COVAXIN
- Viral vector vaccines, which use an altered virus to carry the genetic code (such as DNA) and create a protein that prompts an immune response, without causing COVID-19. For example: COVISHIELD
- mRNA vaccines, which contain “messenger RNA” to make a coronavirus spike protein. This protein alone cannot cause COVID-19.Our cells use this mRNA to make the viral protein that causes our immune systems to make antibodies that fight COVID-19. For example: PFIZER
How to Protect Myself and My Family from COVID-19
What steps can I and my family take to reduce our risk of getting COVID-19?
Practice everyday preventive actions to help reduce your risk of getting sick, and remind everyone in your home to do the same. These actions are especially important for older adults and people who have chronic medical conditions:
- Avoid close contact with people who are sick.
- Wear a mask.
- Stay home when you are sick, except when you need medical care.
- Cover your coughs and sneezes with the inside of your elbow or a tissue, and throw the tissue in the trash. Then wash your hands.
- Wash your hands often with soap and water for at least 20 seconds, especially after blowing your nose, coughing, sneezing, going to the bathroom, and before cooking or eating.
- If you do not have soap and water, use an alcohol-based hand sanitizer with at least 60% alcohol. Always wash hands with soap and water if hands are visibly dirty.
- Clean and disinfect surfaces and objects that people touch a lot (e.g., phones, other electronics, tables, countertops, light switches, doorknobs, and cabinet handles).
- Get vaccinated.
Should I use a facemask or face cover to prevent COVID-19?
UPDATED Everyone, including those who have received the COVID vaccine, should continue to follow COVID appropriate behaviour i.e., mask, do gaj ki doori (physical distance of 6 feet) and hand sanitization to protect themselves and those around from spreading the infection.
You should cover your mouth and nose with a facemask when you are out in public, for example while going to the grocery store. This is to protect others and yourself from the risk of getting COVID-19, since one could spread the virus to others even if they do not feel sick. The facemask should cover the mouth and nose completely. Facemasks must not be shared, and each person should have their own facemasks.
Some masks, like triple layer medical mask and N-95 masks, offer higher levels of protection than others, like cloth masks, and some may be harder to tolerate or wear consistently than others. It is most important to wear a well-fitted mask correctly that is comfortable for you and that provides good protection.
People with COVID-19 and their caregivers should always use a triple layer medical mask. If caregiver and the person with COVID-19 are in same room, both may preferably consider using N-95 mask.
The facemask is not a substitute for social distancing. You should continue to keep 6 feet between yourself and others. Hand washing is still very important, and hands should be washed before wearing the facemask.
Please watch this video by the WHO to learn how to properly fit your mask: https://youtu.be/YPd-XrDhzrQ
For more information, please visit: https://www.mohfw.gov.in/pdf/RevisedHomeIsolationGuidelines05012022.pdf
and
https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/types-of-masks.html
What does it mean to practice ‘social distancing’?
- Keeping your distance from others (6 feet or 2 meters away).
- Not taking public transportation, taxis, or ride-shares during this period.
- Avoiding crowded places (for example: shopping centers, schools, workplaces, movie theaters, and places of worship such as temples, churches, synagogues, and mosques).
How should I clean and disinfect my home in order to protect myself and my family from COVID-19?
UPDATED On a regular basis, clean and disinfect frequently touched surfaces such as tables, doorknobs, light switches, countertops, handles, desks, phones, keyboards, toilets, faucets, and sinks.
After cleaning and disinfecting, clean your hands with an alcohol-based hand sanitizer or wash them with soap and water. Avoid touching your eyes, mouth, or nose.
Adapted from sources: https://www.cdc.gov/coronavirus/2019-ncov/faq.html and https://www.mohfw.gov.in/
For more information, please refer to the revised guidelines for home isolation of mild/asymptomatic COVID-19 cases: https://www.mohfw.gov.in/pdf/RevisedIllustratedGuidelinesforHomeIsolationofMildAsymptomaticCOVID19Cases.pdf
How important is good ventilation to prevent COVID-19 infection?
Ventilation or air flow can help prevent virus particles from gathering in the air in your home. Good ventilation, along with other preventive actions, like staying 6 feet (2 meters) apart and wearing masks, can help keep you from getting and spreading COVID-19.
Ways you can improve ventilation in your home:
- Bring as much fresh air into your home as possible.
Bringing fresh outdoor air into your home helps keep virus particles from gathering inside. Better ventilation means lower chances for transmission.- If it’s safe to do so, open doors and windows as much as you can to bring in fresh outdoor air. While it’s better to open them wide, even having a window cracked open a little can help.
- If you can, open multiple doors and windows to allow more fresh air to move inside.
- Do not open windows and doors if doing so is unsafe for you or others (for example, if there are young children, pets, a risk of falling, high levels of outdoor pollution, or if it could trigger asthma symptoms).
- Filter the air in your home.
- If opening windows or doors is unsafe, think about other ways to reduce virus particles in the air, like using air cleaners and bathroom or stove exhaust fans (see the next 2 points below).
- Learn how to make an air cleaner using a portable fan and cardboard.
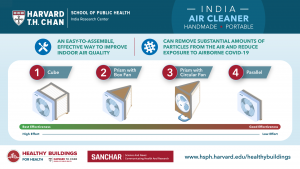
Reduce your indoor exposure to COVID-19. Learn how to make a portable do-it-yourself prism air cleaner with a circular fan to remove contaminants such as viruses from the air.
- Turn on the exhaust fan in your bathroom and kitchen.
- Exhaust fans above your stove and in your bathroom that vent outdoors can help move air outside. You can turn a free-standing fan into an exhaust fan by turning it to face outdoors (to improve air flow outwards).
- Although some stove exhaust fans don’t send air outside, they can still improve air flow and keep virus particles from being gathered in one place.
- Keep the exhaust fan turned on over your stove and in your bathroom if you have visitors in your home. Keep the exhaust fans turned on for an hour after your visitors leave to help remove virus particles that might be in the air.
- Use fans to improve air flow.
- Place a fan as close as possible to an open window, facing outside. This helps get rid of virus particles in your home by blowing air outside. Even without an open window, fans can improve air flow.
- Point fans away from people. Pointing fans toward people might cause contaminated air to flow directly at them.
- Use ceiling fans to help improve air flow in the home whether or not windows are open.
Adapted from: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/Improving-Ventilation-Home.html and https://static.psa.gov.in/psa-prod/publication/Ventilation_PSA_FORPRESS_V1_May19-compressed.pdf
If I have visitors, how can I reduce the risk of spreading COVID-19?
Limit the number of visitors in your home and time spent inside with visitors.
- If you are not sick, and if possible, gather outside in a physically distanced way (stay 6 feet or 2 meters away).
- The more people inside your home, and the longer they stay, the more virus particles can accumulate.
- Limit the number of visitors in your home.
- Be sure that everyone wears a mask over their nose and mouth while visitors are in your home- this includes the visitors and the people who live in your home.
- Try to gather in larger rooms or areas where you can stay at least 6 feet (2 meters) apart.
- Keep doors and windows open for air circulation.
- Keep visits as short as possible.
- Keep exhaust fans turned on and keep them on for an hour after your visitors leave to help remove virus particles that might be in the air. If you do not have an exhaust fan, place a fan as close as possible to an open window, facing outside. This helps get rid of virus particles in your home by blowing air outside.
To understand and determine your risk, visit: https://covid-19.forhealth.org/covid-19-transmission-calculator/
Can COVID-19 positive mothers breastfeed their children?
Yes. Mothers produce antibodies in their milk that will protect the baby and help the baby’s own immune response. This is true whether a mother got COVID-19 before or after delivery. It is advised that she wear a mask while breastfeeding, and wash hands with soap before and after touching the baby.
If a baby is too sick to breastfeed, the mother should express breastmilk and feed the baby with a cup and spoon.
Symptoms, Testing and Treatment of COVID-19
What are the symptoms of COVID-19?
UPDATED The main symptoms of COVID-19 are fever, cough, and shortness of breath or difficulty breathing. Other symptoms include chills with repeated shaking, muscle pains, headache, sore throat, and loss of taste or smell.
People with COVID-19 may also have fatigue (tiredness), nasal congestion (stuffy nose), or diarrhea. However, many people who become infected do not have any symptoms.
Most people who get COVID-19 get better without needing special treatment. However, some become very ill. Please talk to your doctor about any other symptoms that are severe or concerning to you. Please seek immediate medical attention if serious signs or symptoms develop. These could include-
- Temperature more than 100° F for more than 3 days
- Difficulty in breathing or breathing rate >24/ min
- Oxygen level less than 93% on room air
- Persistent pain/pressure in the chest
- Confusion or inability to awaken
- Severe fatigue and myalgia
For more information, please refer to: https://www.mohfw.gov.in/pdf/RevisedIllustratedGuidelinesforHomeIsolationofMildAsymptomaticCOVID19Cases.pdf
Are the symptoms of COVID-19 different in children than adults?
No. The symptoms of COVID-19 are similar in children and adults. However, children with confirmed COVID-19 have generally shown mild symptoms. Reported symptoms in children include cold-like symptoms, such as fever, runny nose, and cough. Vomiting and diarrhea have also been reported. It’s not known yet whether some children may be at higher risk for severe illness, for example, children with underlying medical conditions and special healthcare needs. There is much more to be learned about how the disease impacts children.
Who needs to be tested for COVID-19?
Anyone with symptoms should be tested, wherever possible. People who do not have symptoms but have had close contact with someone who is, or may be, infected may also consider testing – check your local health guidelines and follow their guidance. If you are having symptoms and feel you need to be tested, if at all possible, reach out to a medical provider by phone before seeking care in person.
While a person is waiting for test results, they should remain isolated from others. Where testing capacity is limited, tests should first be done for those at higher risk of infection, such as health workers, and those at higher risk of severe illness such as older people, especially those living in seniors’ residences or long-term care facilities.
For information on Testing Centers in India, please visit:
Map of laboratories- https://covid.icmr.org.in/index.php/testing-facilities
For more information, please visit: https://www.icmr.gov.in/
Which COVID-19 tests are approved in India?
UPDATED There are several tests approved in India to detect the COVID-19 virus. These tests are done with nasal (in the nose) or oral (in the mouth) swabs. The Indian Council of Medical Research (ICMR) has approved the following tests to detect current COVID-19 infection:
Point-of-Care Tests: Home or Self-Test / Rapid Antigen Test (RAT)
MolecularTests: rRT-PCR, TrueNat, CBNAAT, CRISPR, RT-LAMP, Rapid Molecular Testing Systems, Newer SARS-CoV-2 Omicron or variant detection rRTPCR assays
ICMR validated Rapid Antigen Test Kits for COVID-19: https://www.icmr.gov.in/pdf/covid/kits/List_of_rapid_antigen_kits_21012022.pdf
List of COVID-19 testing laboratories: https://www.icmr.gov.in/pdf/covid/labs/COVID_Testing_Labs_26012022.pdf
What should I do if I think I am sick?
If you think you have been exposed to COVID-19, you should stay home and stay away from others as much as possible. If you are sick and develop a fever and symptoms, such as cough or difficulty breathing, call your healthcare provider for medical advice. Many people will be able to recover at home; however, be sure to get care if you think it is an emergency. If you seek care, call ahead to make sure they know you may have COVID-19 so that healthcare workers can protect themselves.
What should I do if someone in my household has COVID-19?
- Prepare a separate room or area for the sick person to stay in, if you can, and keep others away. Keep windows or outside doors open in the room so it’s well ventilated to protect others from COVID-19.
- Pick a household member to be the only person in contact with the sick person. The caregiver should not have contact with people outside the house while anyone inside is sick.
- Reduce contact with COVID-19. Wear a 3-layered medical mask or N95 mask over your nose and mouth. If that’s not possible, double mask (wear a cloth mask over a disposable surgical mask).
- Wash hands often.
- Use separate utensils for the sick person.
- Disinfect surfaces that are touched often, such as, tabletops, doorknobs, and switches.
- Monitor the sick person’s symptoms, temperature and oxygen saturation levels (using a pulse oximeter).
- Pay special attention if the person is at high risk, such as if they:
- are older
- have high blood pressure
- have heart disease
- have kidney disease
- have diabetes
- have other serious illnesses
- Have the sick person rest a lot and drink a lot of water.
- Call a doctor if the sick person has:
- a hard time breathing
- confusion
- loss of speech/mobility
- chest pain
- fall in oxygen saturation levels

Use these tips to keep yourself and your family safe if someone in your household is sick with COVID-19
For more information, please visit: https://www.mohfw.gov.in/COVID_vaccination/vaccination/faqs.html
When should people with COVID-19 stop home isolation?
UPDATED People under home isolation can end the isolation after at least 7 days have passed after testing positive for COVID19, and if they have had no fever for at least 3 continuous days. The person shall continue wearing masks. There is NO need for re-testing after the home isolation period is over.
Asymptomatic contacts of infected individuals need not undergo COVID-19 test. They may monitor health in home quarantine.
For more information, please refer to the revised guidelines for home isolation of mild/asymptomatic COVID-19 cases: https://www.mohfw.gov.in/pdf/RevisedIllustratedGuidelinesforHomeIsolationofMildAsymptomaticCOVID19Cases.pdf
Higher Risk
Who is at risk for serious complications from COVID-19?
People of all ages can become infected with COVID-19, but some people are at higher risk of getting very sick from this illness. This includes:
- Older adults
- People who have underlying chronic medical conditions like heart disease, diabetes, lung disease
This does not, however, mean that other groups won’t fall sick or are immune from it. Everyone is at risk; some more than others.
Are people with disabilities at higher risk for COVID-19 infection or severe illness?
Most people with disabilities are not inherently at higher risk for becoming infected with or having severe illness from COVID-19. Some people with physical limitations or other disabilities might be at a higher risk of infection because of their underlying medical condition.
You should talk with your healthcare provider if you have a question about your health or how your health condition is being managed.
Adapted from source: https://www.cdc.gov/coronavirus/2019-ncov/faq.html#Higher-Risk
What resources are available to me if I am struggling with issues related to sexual or domestic violence during this time?
If there is an imminent danger of violence to you or to someone you know, please contact the nearest police station (police helpline, phone 1091) or the National Commission for Women, Government of India (domestic violence helpline, phone 181).
Pandemics like COVID-19 have a significant impact on individuals, families, and countries. People not only have to deal with the consequences of the disease but also have to deal with the potential consequences of measures taken to contain the disease, like quarantines, social distancing, and lockdowns. Individuals face issues related to health, finances, and security concerns, and these can impact their mental health and their relationships. Since there are curbs on the movement of the individuals, people who are in abusive relationships face greater challenges, as they are likely to be in close confined spaces with abusers and may have difficulties in getting timely help.
UN WOMEN has reported rates of increased violence against women and children (more so girls) during the COVID-19 pandemic. Hence, it is even more important to address this issue, as it can lead to further crisis and possibly secondary trauma.
Source: Mental Health in the times of COVID-19 Pandemic, NIMHANS, https://www.mohfw.gov.in/pdf/COVID19Final2020ForOnline9July2020.pdf
How COVID-19 Spreads
How does COVID-19 spread?
COVID-19, which is caused by the new coronavirus (SARS-CoV-2), can spread from an infected person’s mouth or nose in small liquid particles when they cough, sneeze, speak, sing, or breathe. These particles range from larger respiratory droplets to smaller aerosols (lighter particles that can float and stay in the air longer than droplets, up to three hours).
Current evidence suggests that the virus spreads mainly between people who are in close contact with each other, typically within 2 meters/6 feet. This is why people should keep at least 6 feet distance from others. A person can be infected when aerosols or droplets containing the virus are inhaled or come directly into contact with the eyes, nose, or mouth. Wearing a properly fitting mask can help decrease this risk.
The virus can also spread in poorly ventilated and/or crowded indoor settings. In these cases, aerosols remain suspended in the air or travel farther than 2 meters/6 feet. When possible indoors, open windows and doors for proper ventilation.
People may also become infected by touching surfaces where droplets containing the virus have landed and then touching their eyes, nose, or mouth. Wash your hands with soap and water regularly, and disinfect frequently touched surfaces, such as doorknobs, tabletops, switches, and mobile phones.
Further research is ongoing to better understand the spread of the virus and which settings are most risky and why. Research is also underway to study virus variants that are emerging and why some spread more easily than others.
For more information, please visit: https://www.who.int/news-room/q-a-detail/coronavirus-disease-COVID-19-how-is-it-transmitted
To gain an understanding of COVID-19 transmission in indoor environments, visit: https://covid-19.forhealth.org/covid-19-transmission-calculator/
Can COVID-19 be caught from a person who has no symptoms?
Yes. Infected people can transmit the virus to other people up to 2 days before they develop symptoms. Even if they don’t have symptoms, infected people can be contagious, and the virus can spread from them to other people. And people who develop severe disease can be infectious for longer.
For more information, please visit: https://www.who.int/news-room/q-a-detail/coronavirus-disease-covid-19-how-is-it-transmitted
Are there certain settings where COVID-19 can spread more easily?
Yes, any situation in which people are standing or sitting close to one another for longer than 15 minutes increases the risk of COVID-19 spreading. Indoor locations, especially where there is poor ventilation, are riskier than outdoor locations. Activities where more particles are expelled from the mouth, such as singing or breathing heavily during exercise, also increase the risk of transmission.
The “Three C’s” are a useful way to think about this. They describe settings where COVID-19 spreads more easily:
- Crowded places;
- Close-contact settings, especially where people have conversations very near each other;
- Confined and enclosed spaces with poor ventilation.
The risk of COVID-19 spreading is especially high in places where these “Three C’s” overlap.
Can someone who has been quarantined for COVID-19 spread the illness to others?
Quarantine means separating a person or group of people who have been exposed to a contagious disease but have not developed illness (symptoms) from others who have not been exposed. The purpose of quarantine is to prevent the spread of that disease. A person exposed to similar coronaviruses as the COVID-19 virus usually develops an illness within 10 days of exposure. Because of this, a person who might have been exposed to the virus from another infected person should quarantine themselves for a period of 10 days. During this period, they can develop and/or spread the illness to others. Beyond the quarantine period, the person is considered to be not at risk of developing or spreading the illness.
Mental Health and Well-Being
How do I maintain mental health and wellbeing during COVID-19?
It is difficult to maintain a healthy lifestyle when we are in the middle of a crisis like this. The uncertainty and worries related to finances, childcare, elderly parents, and job security disrupt our routines, our lifestyles, and mental health. The uncertainty about the future, the ceaseless news coverage, and constant social media-driven flood of information and misinformation can increase our sense of anxiety.
Stress is a normal response to these types of situations. Stress disturbs our sleeping and eating patterns, leads to irritability, emotional outbursts, low motivation, and changes in use of alcohol or other drugs. Please do not hesitate to seek help if you are experiencing anything like this. It is also important to have a healthy lifestyle and get back into a routine as much as you can.
For tips to manage stress and promote your mental, physical, and social wellbeing, click the following:
How do I manage mental health during COVID-19 isolation?
Discuss the Importance of Home Isolation
- Explain the importance of home isolation (staying by yourself at home) to those in your home.
- Be clear about how long you need to isolate (remain alone). It is usually for 10 days.
Set a Schedule
- Set a daily routine, including regular eating and sleeping schedules.
- Take up a new hobby, if you feel up to it.
Keep Up a Healthy Lifestyle
- Try to follow healthy habits, including eating well, exercising, and getting good sleep.
- Try not to use alcohol or smoking to cope.
Seek Social Support
- Connect remotely with social networks by phone, online, or other communication channels.
Manage Exposure to Media
- Rely only on credible sources of information, such as the Harvard T.H. Chan School of Public Health – India Research Center or Project SANCHAR
- Avoid constant exposure to negative stories on COVID-19, which may add to stress, anxiety, or panic.
Get Additional Help When Needed
- For help with depression, anxiety, or substance abuse, reach out to a mental health professional through the National Institute of Mental Health and Neuroscience at 080-46110007
How do I maintain the mental health and wellbeing of children during the COVID-19 crisis?
Life in lockdown due to COVID-19 can be particularly distressing for children. With schools closed, children have been staying indoors and missing outdoor activities. Parents are also adjusting to new lifestyles. Many are working from home, some are facing financial challenges, and as parents, they have to attend to their own economic and psychosocial needs, as well as support the health and wellbeing of their children.
While feeling stressed and anxious about the outbreak is natural, the lockdown is also an opportunity to invest in time with your child. Please see the tips below on engaging your child during COVID-19.
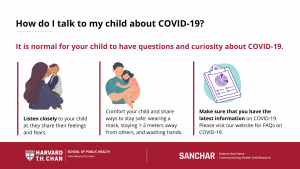
How can I talk to my child about COVID-19?
- It is normal for your child to have questions and curiosity about COVID-19.
- Listen closely to your child as they share their feelings and fears.
- Give your child realistic reassurance, including ways to reduce risk by wearing a mask, staying six feet apart, and washing hands.
- Ensure that you have the latest scientific information on COVID-19. Visit https://www.hsph.harvard.edu/india-center/covid-19-dashboard/ or
How can I support my child during COVID-19?
- Use the lockdown to spend quality time with your child.
- Be responsive to their emotional needs.
- Do not dismiss their COVID-19 worries and fears.
- Set a daily routine for your child, including regular mealtimes and bedtimes.
- Keep your child active and give healthy meals and snacks.
- Lead by example: Practice indoor exercises, yoga, mindful breathing, and healthy eating with them.
When should I seek help?
- If your child shows continued symptoms of heightened stress, anxiety, or difficulty sleeping, consider getting professional help on the government’s Psychosocial Helpline for Children affected by COVID-19, called Samvedna, by dialing “18001212830.”
If any child is in a distress situation, call the “Childline” at “1098” for support.
How do I promote emotional health of my children as schools reopen and they start going back to school in person?
GUIDELINES FOR PARENTS FOR PROMOTING EMOTIONAL HEALTH OF THEIR CHILDREN
- Get the child mentally ready for a new routine: Point out the positive aspects of starting school. Reassure children that if any problems arise at school, parents will be there to help resolve them.
- Be patient: Exercise patience and refrain from using punishment as transitioning once again from home to school may be challenging for the students.
- Encourage children to extend Positive offerings: Children may be asked to draw and color cards for their friends, teachers, and also family members as preparation for school reopening thus setting a positive tone and hope.
- Collect Motivational resources: Students can be asked to collate good audio(podcasts) songs developed for and during the Covid-19 that they find motivating for sharing with school mates
- Ensure their emotional safety: Parents need to make children feel safe and wanted by giving them the feeling that they can share anything and everything with them as they prepare to go to school, as well as their concerns while they are in school.
- Acknowledge their emotions: Stay calm especially when the children are anxious. Pay attention to their feelings and give them space to share their fears, if any. Ensure that there is adequate time for sitting together and talking freely at different times.
- Encouragement: Parents also need to encourage and guide their children to plan their daily schedule for school, studies at home, play, sleep, activities to maintain good health and hygiene, etc.
- Appreciate your child: Recognize and praise even small accomplishments and efforts made by children. This not only develops confidence and self-esteem but will lead to the formation of good habits and better performance in different tasks.
- Set a good example: Before expecting children to be disciplined, empathetic, healthy, and hygienic, parents need to practice such things. Parents need to manage their stress by getting good sleep, exercise, healthy diet, connected with friends and family.
- Acknowledge your feelings: Understanding and recognizing one’s own emotions is vital for one’s well-being. As a parent one can help himself/herself and their children to navigate each one of their emotions and responses.
- Focus on the things that can be controlled: Focusing on things that are out of one’s control can make one feel drained, overwhelmed, and anxious. So, focus on what can be controlled.
- Taking care of the self: Make sure to indulge in physical exercises like yoga. Have a healthy diet and take care of your body.Please visit the website https://mhrd.gov.in/covid-19 of MHRD or avail the tele-counselling services on National Toll-free helpline 8448440632 under the MANODARPAN initiative of MHRD, which provides psychosocial support for mental health and emotional wellbeing of students, teachers and families during the COVID-19 outbreak and beyond.
Source: https://www.education.gov.in/sites/upload_files/mhrd/files/SOP_Guidelines_for_reopening_schools.pdf
Please follow the links below for more information:
Ministry of Health and Family Welfare, Government of India
Indian Council of Medical Research
World Health Organization (WHO) FAQs
CDC Symptom Description and Symptom Checker
CDC Pregnancy and Breastfeeding
Boston Public Health Commission
This material was curated by Viswanath Lab of Harvard Chan School of Public Health and the Dana-Farber Cancer Institute (DFCI) with the help of the Health Communication Core of Dana-Farber/Harvard Cancer Center (DF/HCC). These are not the official views of Harvard Chan or DFCI. For any questions, comments or suggestions reach out to rpinnamaneni@hsph.harvard.edu.